Public Health News
Giving Back

Antonio Herrera ’24 is a public health major in the Falk College who had been involved in the military since 2012, enlisting in the U.S. Air Force and then transferring to the U.S. Army before separating from active duty to pursue his public health degree.
During his time in the military, Herrera traveled all over Europe and Asia, making friends who helped him learn different languages. He discovered a love for languages, culture, and traveling, so when he heard about the English Conversation Group through Syracuse University’s Center for International Services, he knew he wanted to assist others who were in the same situation that he had once been in.
Learn more about Herrera’s role as an English Conversation Group facilitator and how you can get involved in the conversations in this story from Syracuse University News.
Welcome from the Dean

Dear Falk Students,
It is with great excitement that I welcome you to campus as we start the fall semester. Like many of you, I am new to Syracuse and look forward to learning all that I can about this amazing institution, I encourage you to do the same. A special welcome to the Class of 2027 and our new transfer and graduate students. We are thrilled that you have joined the Falk College family and we look forward to working with you as you pursue your academic and professional goals.
As classes begin, I want to remind you of resources on campus that will help you succeed.
Official Syracuse University Communications
Syracuse University email is the primary communication method at the University. Your professors and University offices will contact you with important information using your Syracuse University email address (ending in “@syr.edu”), not your personal email address. It’s important to read your University email at least once every day so you’re aware of the latest information that’s essential to you.
Student Support Services
Falk College Student Services is an important resource in your support system at Syracuse University. Student Services counselors are here to provide you with academic advising and help you meet your requirements and goals. In addition, they are your resource for private consultation related to student social and emotional concerns. If you have any concerns throughout your academic career, please contact Student Services or visit Falk 330, Barclay Suite in the Falk Complex.
I encourage you to connect with the staff at Falk Career Services, who can help you prepare for life after college through career exploration, internship and job searching, professional networking, and more. They are also located in Falk 330, or you can search for opportunities through Handshake, the University’s job search and professional events portal.
In addition, you can connect to spiritual life on campus at Hendricks Chapel, as well as health and counseling services in the Barnes Center at the Arch.
Student Spaces in Falk College
The Student Lounge, located in Falk 216, is available to you anytime the Falk Complex is open. The lounge has a microwave, refrigerator, and vending machines for student use. Across the hall is the Falk Café on 2, open 8:00 a.m. to 3:00 p.m. Monday through Friday starting August 28. Visit the Food Services website for up-to-date operating hours for cafés and dining centers across campus. Just down the hall is Falk 229, the quiet student lounge.
There are several computer labs in the Falk Complex. Falk 113 is a PC lab, and Falk 229 is a quiet study area that has both PCs and Macs available for your use. Both spaces are available to students at any time. Falk 400 and 407 are PC labs that are also used as teaching classrooms. When class is not in session, they are open for student use. You may check their schedule of availability using the 25Live website. You may also use the quick-print stations in Falk 216 and 229 for printing and email. These stations log out automatically after 10 minutes of use.
Ways to Get Involved
The Student Involvement Fair will be held Thursday, September 14 from 11 a.m. to 2 p.m. on the Quad. There are more than 300 student organizations at Syracuse University. Be sure to explore organizations that might be outside your usual interests, too. Remember, this is a great way to meet new people and discover something new about yourself!
There are many exciting events planned for Fall 2023, including two signature Syracuse University events: Family Weekend November 3-5 and Orange Central, Syracuse University’s annual homecoming and reunion weekend, September 28-October 1. You can discover activities and events on campus by visiting the Syracuse University Calendar.
There are countless ways to get involved at Syracuse University, and these are just a few suggestions to get you started. I encourage you to visit syracuse.edu/life/students for more resources and opportunities to make the most of your Syracuse experience.
All Falk students are invited to join me and Falk College faculty and staff for refreshments in Falk 335 during meet-and-greets on Wednesday, September 6 from 10 a.m. to 12 p.m. and Thursday, September 7 from 10:30 a.m. to 1 p.m. We hope to see you there.
I wish you every success on your journey here at Falk College. I am eager to see all the ways in which you will become part of—and add to—the Syracuse community.
Go Orange!
Jeremy S. Jordan, Ph.D.
Dean, Falk College
Welcome to Falk College!

Syracuse Welcome, the University’s required orientation program, is scheduled for Aug. 24-27. At Falk College, we’ll be welcoming a student body that includes more than 2,100 undergraduate and graduate students.
The newest Falk students in the Class of 2027 are a talented group from 31 U.S. states and 10 global countries. Joining the Falk family are 319 first-year students, 16 transfer students, and 283 graduate students (123 in residential programs and 160 in online programs).
For everything you need to know about Syracuse Welcome, please visit the Welcome Schedules webpage, where both University and Falk College-specific events can be found. Welcome to Falk College and Syracuse University!
Together for Better: Diane Lyden Murphy’s 45 Years of Service

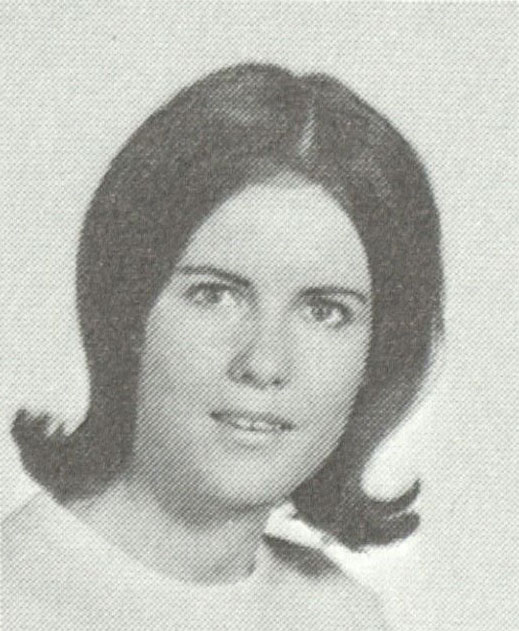
Many know Diane Lyden Murphy as the Dean of Falk College, a position she has held since 2005. But her journey and impact at Syracuse extend well beyond her deanship. In many ways, her leadership in Falk College was shaped by the people and experiences in Diane’s life before Falk College even existed.
As we approach the end of August 2023 and the conclusion of her deanship, we sat down with Diane to reflect on her personal journey to academia; her calling to social policy, social justice, and feminist scholarship; and her remarkable 45 years of service at Syracuse University. Here is her story:
Moving In a Crowd
“Do you want to be a jumping hyena? Or do you want to play ball?” One of the sisters who taught at Our Lady of the Valley, a Catholic high school in Orange, New Jersey, was encouraging a young Diane Lyden to join the basketball team. It was the early 1960s, a time when women’s competitive sports were still new and most young women were cheerleaders. “The nuns were my first feminist teachers,” she said. “I didn’t know it then.”
Thanks to the nuns’ encouragement, Diane joined the women’s team, which won several state championships in northern New Jersey. “I wasn’t top of the team. But my very best friend Bernie was. She was a top shooter in Jersey. Boys would get scholarships every year. But there were no scholarships for Bernie, so she did not go to college.”
Growing up in North Jersey, there were Irish, Italian, and Polish neighborhoods. At home, she was part of a multi-generational household of first-generation Irish Catholics. Diane was the eldest of 10 children—four girls and six boys. The house was huge, and it needed to be—it was home to her siblings, grandparents, and aunt and uncle “I’ve always lived in a gang, that’s how I moved around and knew life. There were always little kids around. There was always lots of activity. We went to school, and church, and athletics. You had to do well in your own role.”
In school and at home, Diane found a mix of “old world” culture mixed with the social justice values of her Jesuit education and home upbringing. “The whole ethos and modeling and life I had was always built around issues of social justice and giving back and philanthropy, mutual aid, and leadership in that area. The concept that what you’re given must be returned,” she said.
The family went to mass every day, and they all worked by the time they were 16. “I either volunteered, or by 16 I had a job.” In high school, Diane was a hospital volunteer, often called a “candy striper.” Even there, Diane was marching to her own drum. “I kept getting into trouble because I kept on serving the people. You’re supposed to just give them their food and leave—but I kept on feeding the old people,” she said, grinning. “The nurses finally said to me, ‘You’re only supposed to leave the trays, you’re not doing the right job, you’re fired,’” she laughed. “I had a little rebel streak. If anybody said don’t, I did.”
But as traditional and new ideas of the world in the 1960s found themselves at odds, Diane found a way to preserve the best of both and still push for progress. Perhaps her biggest act of individual thinking was her decision to go to college. Diane had a knack for academia; she took three years of math, and even won a state award for her four years of Latin language education.
Although she was at a college prep school, her family did not understand why she wanted to go to college. No one in her family had earned a bachelor’s degree, and the women didn’t receive any college education. Money for higher education was reserved for the men in the family. Her father, an Irish biological orphan raised by an adoptive Polish family, had an associate degree and a stable white-collar job in traffic control. Just as Diane was finishing high school, her father was being transferred to Upstate New York. Since her family was relocating to Syracuse, Diane enrolled at Syracuse University.
A Born Social Worker
Diane became part of the progressive action movement in the community and on campus. “It was a social activist time. It completely meshed with my own mission and values. So, I became an activist scholar.” She majored in sociology at the Maxwell School and was part of the honors program. At the time, social work was not an undergraduate major.
“My parents didn’t help me financially because they couldn’t. I always worked. I worked at the bookstore, lifeguarding, water safety. I worked all through college. I did my schoolwork at home at night.” As an undergraduate student, Diane lived with her family in a big farmhouse. She shared a room with her two sisters. Second in birth order was Diane’s sister, who was following a more traditional path. And while her grandmother gave her sister a dowry, Diane only wanted books. “Grandma would say, ‘Any money I give you will not go into a book!’ It was so far from her experience as a farm child in the Catskills.”
As a senior, she received her honors degree in Hendricks Chapel. “My parents came for the first time to campus, and my father said, ‘What are you doing?’ Meaning, ‘What is this all about?’ My family always loved me and supported me, but, having never experienced it themselves, did not understand higher education.” Although her family did not understand Diane’s chosen path, she credits them with setting her on it. “My inclination to social justice comes out of my early preparation as a child. My parents showed the way,” she said. “All my brothers and sisters do this work. We’re all involved in human services: Doctors, healthcare workers, lawyers, social workers, teachers, and on and on it goes.”
While at Syracuse, Diane met Fred Murphy, a graduate student in economics at the Maxwell School, five years her senior. “He was also an activist scholar. He was employed by the City of Syracuse doing tenant organizing.” One week after her graduation in 1967, Diane and Fred were married. In January 1969, their twin daughters were born.
No Stopping Her
Diane was working at Elmcrest Children Center with a team of six women, each of whom had their Master of Social Work. “You’re a born social worker,” her supervisor told Diane. After a year at Elmcrest, she made her way back to Syracuse to earn her own M.S.W.
Diane arrived at the admissions office with her twins and was greeted with a comment she’d never forget: “‘What are you doing with those babies sitting in my office for admissions?’ he said to me. ‘I’m applying to graduate school.’ ‘And what makes you think that’s reasonable, young lady?’ I said, ‘Because women do it all.’ I was so upset, it got me charged up. I said to myself, ‘I’m really going to do this!’”
She started courses in social work in the fall of 1969. “By this time there was no stopping me. I really loved my studies in social work.” At the time, her twins were not yet 1 year old. There were no childcare services on campus for students with children, and since Fred was working full time, they went to class with Diane. “I took them to school. I brought them to class,” she said. “Still to this day my friends from graduate school talk to me about holding them on their lap. I often rode on a bike with them—one on the front and one on the back. It was a little challenging, but all my friends I met in class helped me do it.” In the M.S.W. program Diane became president of the social work Graduate Student Organization.

Diane paid for her education through scholarships and teaching assistant stipends. These turned into formative experiences for her. “I was given the opportunity to make family-friendly structural changes for all members of the university community, working side-by-side with mentors, university leaders, and countless collaborators.”
In her first year as a graduate student intern, Diane worked with Central New York Legal Services in local family court cases. In her second year, she worked with Dr. Charles Willie, then-Dean of Student Affairs and previous chair of the sociology department whose research focused on mental health in African American families. “That was an unbelievable adventure working with him as his graduate assistant. What a privilege. He ended up being tenured at Harvard University’s School of Education. Under his mentorship, we developed and founded the Syracuse University Early Childhood Education Center.”
By the early 1970s, there was a large population of married students and families, many of whom were having children. But there were only minimal health benefits at Syracuse University. The Family and Medical Leave Act (FMLA) was more than 20 years away. “Dr. Willie said to me, ‘Married students are a poverty population.’ And they were.” And although Syracuse University had the Bernice M. Wright Laboratory School, the school was a cooperative model, and it didn’t take infants. Together, Dr. Willie and Diane as his graduate assistant established the Early Childhood Education Center funded between the Department of Psychology, the School of Education, and the Office of Student Affairs. They also created a program with SUNY Upstate Medical University to help students access affordable childbirth delivery.
After completing her M.A. social science in 1976 and her M.S.W. in 1978, Diane decided to continue with a Ph.D. “Obviously I was kind of pushing against things all along, and now it became pretty obvious what the mission was. There’s no question of the intentional effort that we would make this university a model for family friendly policy.”
Trained by the Very Best
Throughout her doctoral studies, Diane worked with Dean of the School of Education Burton Blatt, Doug Biklen, Bob Bogdan, Steve Taylor, and other scholars and partners at the Center on Human Policy in the School of Education. “These were the School of Education’s flagship signature moments, and we were the literal pipeline of funding from Washington. Most of the federal funding for the nation came to Syracuse University for disability studies.” In part, the Center worked on deinstitutionalization and the promotion of community care models. “This was a big part of my journey in my 30s and 40s and this movement in disability studies transformed America,” she said.
Diane’s colleagues at the Center were trailblazers for inclusive education. The Jowonio School was an early pilot of inclusive education modeling that was created by the School of Education. They integrated these models into the Early Childhood Education Center and the Bernice M. Wright Laboratory School before they became the model for the surrounding Syracuse community, and eventually the world. “Now inclusive education is mainstream. Syracuse University School of Education built that,” she said. “I am pleased to say every one of my children have been educated within an inclusive education environment. It makes a world of difference, and everyone benefits.”
All of Diane’s doctoral work was done with the Center on Human Policy. In her graduate assistant office on campus, she kept a crib for the twins where they would sleep while she wrote her dissertation.
She earned her Ph.D. in 1983 and by then, Syracuse University was truly her home. “I had a lot of good fortune,” she said. “I had been trained by the very best and got to do the work I love, which is organizing and planning social change, having the university engage in the community and the community engage in Syracuse University.” She loved academia, and she felt part of the community. And perhaps most importantly, she could see an opportunity to make change in the place she had grown to call home. “I realized I could do activist organizing within the university community and make this a better place for all,” she said. “So, I stayed, and I never left.”
Together You Create the Shift
As a member of the University Senate since 1979, Diane was deeply involved in writing new policies for the university. She and her colleagues formed policies for women’s concerns, gender pay equity, and sexual harassment. They established benefits for parental leave, adoption, domestic partnerships, and retirement. “We looked across the nation and even in Europe to see what best healthcare policies to have at a university. We adapted them, we brought them in, we pushed for them. You have to be strategic and skilled in community change and movement and organization theory—and we were. So, we’ve attended to all those things and we’re a better place because of it.
“But we can’t rest on this,” she continued. “Although there has been accomplishment, we realize there is a harsh political context to consistently work in. But the university has been responsive through its legislative and statute process, through the University Senate, our chancellors, and our provosts, and community leaders have been responsive to working towards a progressive site. That’s a gain for the entire community.”
Active in the early women’s movement in the wider community, Diane was one of four charter members of The Women’s Center, which operated consciousness raising (or “CR”) groups in Syracuse and surrounding towns. It’s still active and located on Allen Street and Harvard Place. From 1993-1994, Diane served alongside her colleague Dr. Marie Provine, a lawyer and Chair of the Department of Political Science, as consultants to Chancellor Kenneth Shaw on women’s issues.

In 1989, Diane took on a new role establishing women’s studies at Syracuse University. She recalls university leadership asking, “Why do we need women’s studies?” “Because everything else is men’s studies,” she said. She was Director of Women’s Studies for more than 16 years. Together with her colleagues, they established women’s studies as a department in the College of Arts and Sciences, and created a major, a minor, and a certificate of advanced study. “Women’s studies is an articulation of giving women the opportunity to study every subject through the lens of women and their history and contributions. It shifts the perspective by focusing on women in all academic fields. And it has created the movement of women’s perspective entering every field of knowledge without exception. This perspective is not yet universal, and there is more progress to be made,” she said.
“You do that collectively,” she continued. “Collectively means you have women that are interested in doing this and leading this as mentors in every possible place in the university and community, and together you create the shift in knowledge.”
Following Dr. Claire Rudolph and Dr. Nancy Mudrick, Diane in 1978 became the third female faculty member to join the School of Social Work. She taught macro policy and law in mental health and developmental disability policy, emphasizing the importance of building change into structures, processes, and systems. “I know as an organizer, until you build it into the structure, it goes with the wind.” She loved teaching her students how to work with people to make progress–something she’s been doing her whole life. But perhaps her biggest challenge was yet to come.
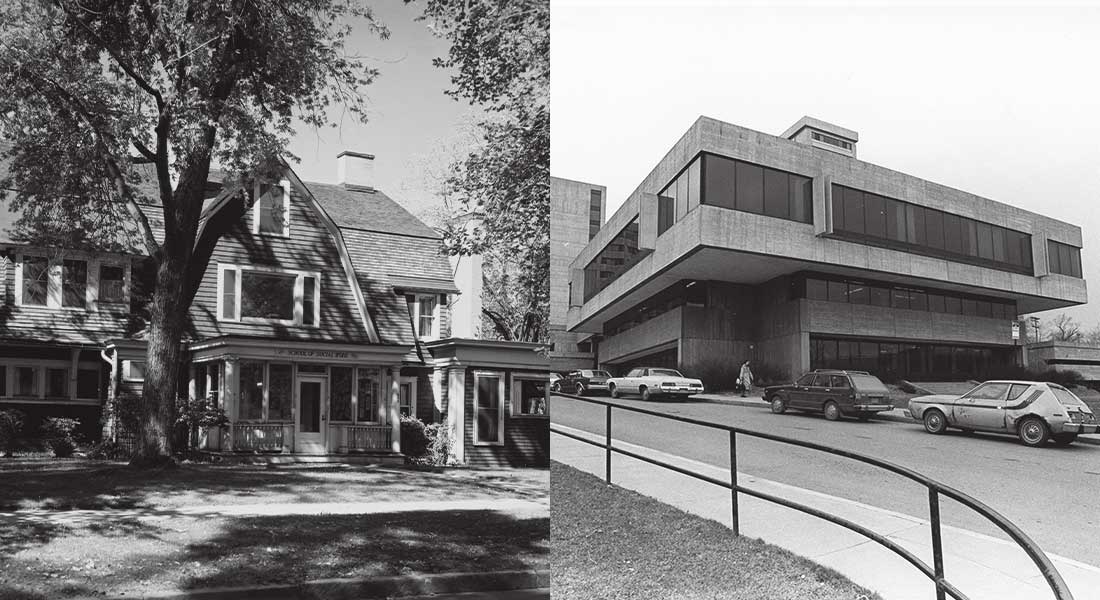
We’re Going to Build It
In 2001, Syracuse University merged the College for Human Development, the School of Social Work, and College of Nursing together to form the new College of Human Services and Health Professions (renamed the College of Human Ecology in 2007), led by Dean William Pollard, former Dean of the School of Social Work. The merge raised questions from faculty about the future of their programs. What does it mean for the formerly independent disciplines? How would the programs continue as a collective College? “It was a challenging time,” said Diane.
In the fragile early years of transition, the university began a search for Pollard’s successor. Although a dozen candidates were vying for the job, Diane wasn’t one of them. But the university leadership identified her as a strong candidate, thanks to her track record of success in leadership and community organizing. She was heavily recruited. Still, many of the university’s leaders openly expressed their doubts about the ability of the college to succeed. She recalls a conversation with one member of university leadership who said, “If I were you, I would take the job and let it fall to its own because it’s never going to work. Let it fall apart and that’ll be the end of it.”
Even Diane had her doubts. But taking the job under the assumption of failure was unacceptable to her. She would accept the job under only one vision: that it would succeed. “I remember saying to myself, ‘If I’m going to do this, we’re going to do it! If these schools must be arranged like this, then we’re going to build it so that we can live and thrive in this structure. Otherwise, all the programs will go away.’ And that’s what I said to the committee: We’re going to build this thing.” In 2005, she was selected unanimously by full faculty vote.

For Diane, failure wasn’t an option. The programs themselves—professional programs in health, nutrition, social work, human development, and others—were too vitally important to society in promoting health and equity. “I said to the faculty, ‘We’re going to take this College and make it what we want it to be. What we know it is. But we will do it. We won’t let it fail because our subject matters are too important. We can do this together—and we will do this together.’”
Diane was the perfect choice to join people together to create a new community. “I was raised in a crowd from the time I was a young person in a large family. I move in a crowd.
“I never make decision alone,” she continued. “I assume that I have other experts around me—we bounce off ideas, we have discussions, and we come to collective work that I think represents the best of everyone. And that’s guided me even to the deanship.”
As the College structure was being formed, so was its identity. With Diane at the helm, the college was built on the principles of social justice and civic engagement. It became a college where putting theory into practice is about more than just gaining practical experience, but about serving others and fostering humility and understanding in diverse global cultural contexts.
Among the merged colleges was a curriculum for sport management, written by faculty in consumer studies, one of the academic programs that had been newly introduced as part of the merge in 2001. In 2004, Falk College launched sport management built on the framework of social justice and corporate social responsibility. In many ways, a socially minded business program was ahead of its time. But the students embraced it, and since 2006 they have raised more than half a million dollars for local charities and continue to lead discussions about diversity and equity in sports.

With support from Syracuse University alumni David Falk ’72 and Rhonda Falk ’74, the College was renamed the David B. Falk College of Sport and Human Dynamics in 2011. The Falk College Complex, former home of the College of Law, was dedicated 2015. Falk programs which had been dispersed in eight different locations across campus were finally all together under one roof. “It’s 18 years since I became Dean, and we have built it. We are a huge success on every dimension,” she said. “We’ve done it as a collective. We’ve done it as a community.”
Today, Falk College boasts impactful interdisciplinary faculty research in human services, health, and social equity. The curriculum integrates highly effective theory-to-practice learning models for student training. Falk College created new undergraduate and graduate academic programs in food studies, esports, and sport analytics at Syracuse University, new programs public health from the legacy of the former College of Nursing, and new programs in exercise science which began in the School of Education. Students also benefit from new global study abroad programming across Europe, Asia, and Africa.
But most importantly, every year the College graduates a cohort of students who are prepared to make their communities stronger, healthier, and more just places. “When students come and study in Falk College, they’ve already made decisions about what they want to do in their life. They want to be largely involved in improving the lives of others through their professional career. They bring such joy, commitment, eagerness, and innovation. That’s the everyday lift you get from being around Falk students.”

Accomplishment in Doing Good
Diane recalls words from a colleague and friend who said to her, “I have never seen anybody fight so hard and forget so easy. You can work with anybody.” She has grown to be admired for her ability speak truth to power in a way that maintains respect and preserves unity.
“I have an ungainly and probably not grounded sense of self confidence, and still do to this day,” admitted Diane, a self-described “straight-shooter.” But she is still inclined toward a bit of humor. Empathy and humility have been guiding principles in her life and leadership. “I don’t feel above anybody else, and I always value diverse perspectives,” she said.
For the campus community, Diane’s legacy will be her effectiveness as an advocate for change and her ability to move groups of people together for better. “It’s a sweet and lovely feeling of accomplishment in doing good.”

But for Diane, her legacy is the one she shares with her late husband, Fred: Their five daughters, their grandchildren, and their commitment to their communities. “I am certainly a feminist. I get it right back at me now from five feminist daughters of whom I am immensely proud.” All her daughters work in education, health, and helping professions. All are heavily involved in civic activity, and not by accident “Fred and I raised our family in the City of Syracuse by determination. We’re urbanists.” Still today, Diane is a proud member of the Westcott community.
Over the years, Diane’s big family home just kept getting bigger, encompassing her family, her Syracuse neighbors, and the university community. “I feel privileged to have had the chance to practice my own values, my own mission, my own journey as I saw it with my family. To be able to execute that and to live that life comfortably and bring that to work, I mean, what an opportunity. I get to work every day at what I love to do. It is quite a privilege and I know that.”
Thanks to Diane and the progress she helped forge in favor of social justice, more people can enjoy that same privilege of shaping their own path in life and living out their own personal mission in all circles of influence–at home, at work, and in the community–instead of having to choose. After all, if Diane has demonstrated one consistent truth, it’s that change can only be achieved if it is achieved together.
Story by Valerie Pietra. Special thanks to Matt Michael for editorial collaboration and contributions and Syracuse University Archives Special Collections Research Center for research and photography.
Kay Stearns Bruening Appointed Associate Dean of Falk College Academic Affairs

Kay Stearns Bruening, Ph.D., RDN, FAND, associate professor in the Department of Nutrition and Food Studies in the Falk College, has been named Associate Dean of Academic Affairs for Falk College effective August 1, 2023. In her new role, Bruening oversees program review, curriculum development, and accreditation for Falk College academic programs.
Previously, Bruening was an undergraduate director in the Department of Nutrition and Food Studies and director of the Nutrition Assessment, Consultation and Education (ACE) Center. Bruening has also served as a program reviewer for the Accreditation Council for Education in Nutrition and Dietetics (ACEND) for 21 years and as a Program Representative on the ACEND Board. Most recently, Bruening was instrumental in Falk College’s early transition to ACEND’s Future Education Model and the successful accreditation under these new standards. This was a multi-year effort that started in 2019, when Syracuse University was accepted as a demonstration cohort to participate as a pilot program of ACEND’s vision to implement competency-based learning to prepare nutrition and dietetics professionals for future practice.
“Falk College is highly regarded for our curriculum, pedagogy, and student success,” says Bruening. “Throughout the college, our curriculum blends theory and research with practical experience, preparing our students for leadership and innovation in critically important professional fields. I am thrilled to serve in this new capacity as Associate Dean and advance Falk College as a leader in education and professional practice.”
Employment outcomes for all majors and the ability of students to seek additional educational goals are excellent throughout Falk College. Accredited programs and license-bearing degrees have an outstanding level of success. Falk College meets, and often exceeds, standards for four accrediting bodies: Accreditation Council for Education in Nutrition and Dietetics, Commission on Accreditation for Marriage and Family Therapy Education, Council on Education for Public Health, and Council on Social Work Education. Falk’s professional programs are consistently among the nation’s strongest in licensing exam pass rates.
“Kay brings a wealth of expertise in educational instruction and design,” says Diane Lyden Murphy, M.A., M.S.W., Ph.D., Dean of Falk College. “Her work in the Department of Nutrition and Food Studies has kept this program at the forefront of nutrition and dietetics education, as evidenced by our accreditation and favorable licensing exam pass rates. Falk College is privileged to have her leadership in a new capacity as Associate Dean.”
Bruening’s teaching and research interests center around medical nutrition therapy, and she is published in dietetics education. She has collaborated with international dietetic education programs in Chile, South Korea, Qatar, and the United Arab Emirates, and collaborates with local medical researchers on detection of adult malnutrition and developing food-based programs for adult weight management and related comorbidities. She is a Fellow of the Academy of Nutrition and Dietetics, belongs to three dietetic practice groups, and completed advanced training in child and adolescent weight management. She holds a courtesy faculty appointment with the Department of Medicine at Upstate Medical University, where she is a co-instructor on an elective nutrition course for medical students.
She earned a Ph.D. in clinical nutrition from New York University, M.A. in nutrition from Syracuse University, and B.S. in biology from St. Lawrence University.
Kay succeeds Eileen Lantier, R.N., Ph.D., who is concluding her 17-year tenure as Senior Associate Dean of Faculty, Curriculum, and Alumni on August 24, 2023. Under Eileen’s leadership, Falk College has successfully launched a wide range of new residential and online academic offerings, sustained accreditation with its four accrediting bodies, and achieved remarkable student outcomes from its signature theory-to-practice model.
Eileen has served more than 39 years at Syracuse University as a faculty member and administrator. Prior to her role as Senior Associate Dean in Falk College, she taught nursing at Syracuse University and championed the use of educational technology in healthcare. Prior to her work in academia, she led a professional career in nursing, working in several area hospitals and clinical settings. She earned a Ph.D., M.S., and B.S., all from Syracuse University. Eileen will retire in January 2024.
“I have served with Eileen since the very beginning of my deanship in 2005. Eileen has demonstrated extraordinary leadership to the great benefit of Falk College and has been instrumental both in developing new academic disciplines at Syracuse University–such as public health, food studies, and sport management–and maintaining excellence and accreditation in our longstanding professional licensing programs,” says Murphy. “Falk College thanks Eileen for her service and lasting positive impact at Syracuse University, her passion for excellence in education, and her deep personal commitment to our students and their success.”
At the end of August 2023, Murphy concludes her tenure as Dean of Falk College, a position she has held since 2005. She is succeeded by Jeremy S. Jordan, a seasoned academic with extensive experience in sport and recreation management. Jordan’s appointment as Dean of Falk College begins September 1, 2023.
Jeremy S. Jordan Named Dean of Falk College

Jeremy S. Jordan, a seasoned academic with extensive experience in sport and recreation management, has been named the next dean of the David B. Falk College of Sport and Human Dynamics. The announcement was made today by Vice Chancellor, Provost and Chief Academic Officer Gretchen Ritter. His appointment, effective September 1, was approved by the Executive Committee of the Board of Trustees.
“Jeremy Jordan brings a combination of academic leadership experience and hands-on industry knowledge that will be a boon to Falk College and its professional programs—from food studies to marriage and family therapy to social work,” Provost Ritter says. “I look forward to working with him, especially on important initiatives like the launch of the esports degree and the expansion of the sport management program.”
Jordan is currently the vice provost for faculty affairs at Temple University in Philadelphia, where he is also a professor and Ed Rosen Senior Research Fellow in the School of Sport, Tourism and Hospitality Management’s Department of Sport and Recreation Management. He is the NCAA Faculty Athletics Representative, and has also been the director of the Sport Industry Research Center and the Millard E. Gladfelter Research Fellow.
Jordan’s research focuses on the impact of sport participation and events on individuals and communities, as well as the social, environmental and financial impact of sport events and organizations. He has authored numerous peer-reviewed articles and book chapters, and has participated in more than 65 funded research projects.
Before joining Temple in 2008, Jordan held faculty positions at the University of Miami, Mississippi State University and the University of Memphis, and served as the athletic director at La Sierra University in Riverside, California. He earned a Ph.D. in sport management from The Ohio State University, a master’s degree in exercise and sport science from the University of Utah and a bachelor’s degree in physical education from La Sierra.
“I am honored to have been selected as the next dean of Falk College and look forward to becoming a member of the Syracuse community,” Jordan says. “The college is known for its academic excellence, impactful research and commitment to community engagement. I admire the culture and rigor of the college and Syracuse University, and I look forward to contributing to the success of both with the support of the students, staff, faculty and alumni.”
The dean search committee, convened by Provost Ritter in February, was co-chaired by Falk College faculty members Mary Graham, professor of sport management and faculty athletic representative, and Katherine McDonald, associate dean of research and professor of public health.
“I am grateful to the committee members for their hard work in recruiting a talented leader like Jeremy Jordan to join our campus community,” Provost Ritter says.
Jordan succeeds Diane Lyden Murphy, who is concluding her tenure as dean of the Falk College, a position she has held since 2005. She has served 45 years at Syracuse University. “Diane has truly left her mark on Falk College, shepherding it from its early days and overseeing multiple successful initiatives,” Provost Ritter says. “I thank her for her service and her incredible contributions to the college and the University.”
First Of Its Kind

A new study led by Falk Family Endowed Professor of Public Health Brooks Gump and published in the journal JAMA Network is the first research to directly measure the associations between arsenic exposure and precursors to cardiovascular disease in children.
A new study led by Falk Family Endowed Professor of Public Health Brooks Gump and published in the journal JAMA Network is the first research to directly measure the associations between arsenic exposure and precursors to cardiovascular disease in children.
The research team considered arsenic exposure and health data of 245 children in the Syracuse, New York, metropolitan area. The study’s findings are important because they highlight the need to reduce arsenic exposure in children.
In this Q&A with Syracuse University News, Gump shares details about how this research can contribute to safer public health standards, and how arsenic exposure in children potentially accelerates the development of cardiovascular disease in adults.
SHE-CAN Scholar

Run, Sreynoch Van ’26, and Pisey Kim ’26 all went through a highly rigorous and selective process to become SHE-CAN (Supporting Her Education Changes A Nation) Scholars. They are striving to develop professional skills at Syracuse to take home to Cambodia, hoping to inspire young women and children to follow in their footsteps.
To learn more about how the Tree of 40 Fruit on the Syracuse University campus spurred Run’s intrigue in studying at Syracuse and what she plans to do when she returns to Cambodia, read this story about the SHE-CAN Scholars.
Congratulations Class of 2023

Along with Dean Murphy, the entire Falk College community of students, faculty, staff, alumni, community partners and friends, congratulates to the Class of 2023! Falk College’s seven academic departments and schools represented 529 degree candidates, including:
- 321 undergraduates;
- 155 masters candidates;
- 50 students earning certificates of advanced study, and;
- 3 Ph.D. students.
Through the month of May, departments across Falk College honored student achievements and celebrated the graduating Class of 2023, which are detailed on individual department websites.
Falk College Convocation was held Saturday, May 13 at Lally Athletic Complex. Falk College Convocation, other college convocations, and the May 14 Syracuse University Commencement ceremony, were recorded and are available to view on the Syracuse University commencement website and is also included below.
Falk College Convocation | Saturday, May 13 | 5:30 p.m. ET
Syracuse University Commencement | Sunday, May 14 | 9:30 a.m. ET
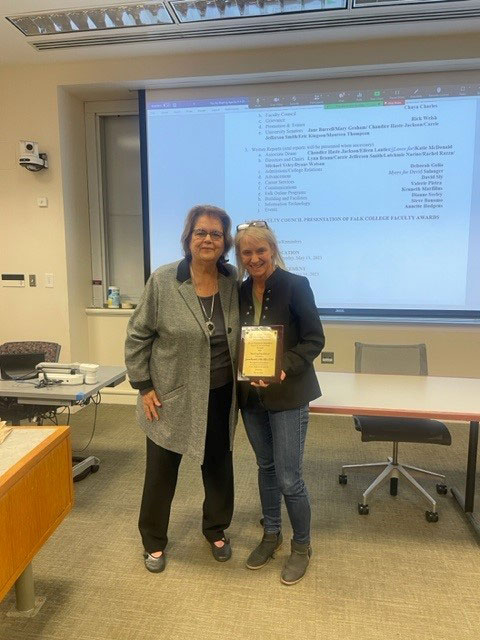
Faculty of the Year Awards
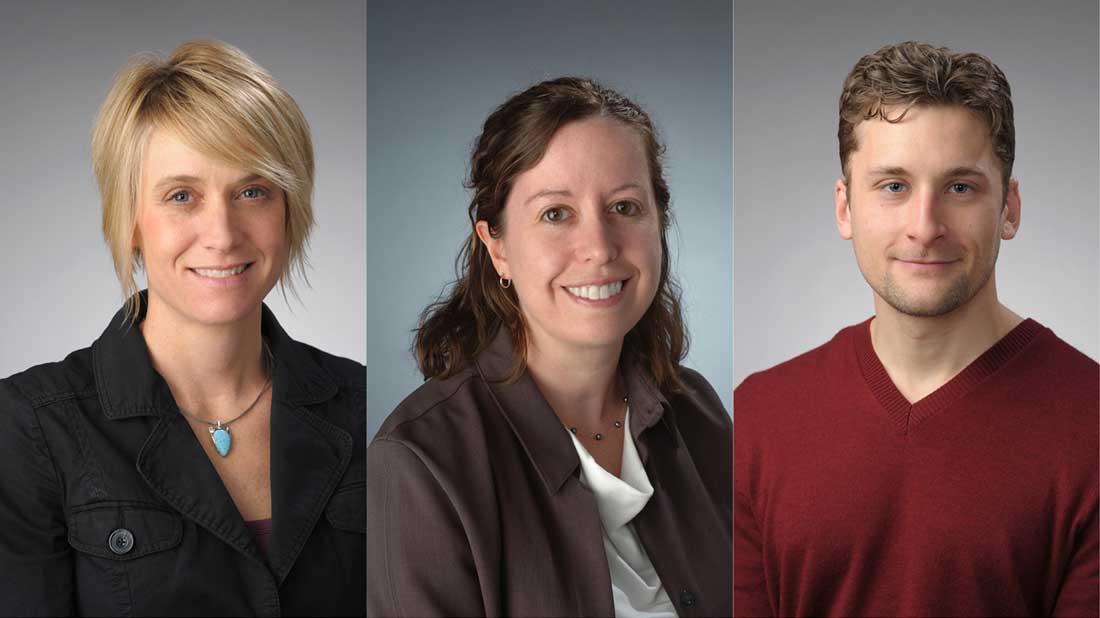
Jane Burrell, Lynn Brann, and Bryce Hruska were honored with 2023 Falk College Faculty of the Year awards for excellence in teaching, service, and research, respectively. The honorees were nominated by their peers for outstanding teaching, scholarship, and internal and professional service contributions and announced by the Falk Faculty Council in early May.
Chaya Lee Charles, an assistant teaching professor in the Department of Nutrition and Food Studies and chair of the Falk Faculty Council, thanked all faculty members who submitted nominations and her fellow Faculty Council members for their time and efforts in the award selection process.
“It is inspiring to see the talent and excellence that we represent as a college, and the high caliber of the nominees made our job challenging,” Charles says. “The Faculty Council is excited to share the results of our thoughtful deliberations.”
Here’s a look at the 2023 honorees with comments from their award presenters:
Jane Burrell
Associate Teaching Professor in the Department of Nutrition and Food Studies
Evan Weissman Memorial Faculty of the Year Award for Teaching Excellence
From presenter Lisa Olson-Gugerty, associate teaching professor in the Department of Public Health:
“Jane has taught and continues to teach multiple courses in her department, and her teaching prowess was described as dynamic and responsive to her students’ needs. Her ability to teach with such excellence stems from her lengthy past and current clinical work in nutrition and dietetics. In other words, she is teaching from ‘hands-on’ experience.
“Jane has mastered adaptability in the classroom. She teaches introductory nutrition (NSD 225) in multiple modes, modifying delivery and assessment to match her audience. In the fall, Jane teaches a large section of NSD 225 for students from across campus. Given the size and limited support (10 teaching assistant hours per week), managing NSD 225 requires organization and attention to detail. Jane keeps the class current by modifying content, utilizing new textbooks, and adopting technology to engage a large audience.
“Jane is dedicated to professional development. In 2022, she participated in a Peer Teaching Evaluation Workshop focused on ‘Small Teaching,’ a book James Lang. She utilized this new knowledge in her ‘NSD 342: Nutrition in the Lifespan’ course. She initiated low-stakes quizzes, providing immediate feedback and a sense of where students stood in the learning process. Jane further modified NSD 342 after attending the Equity-Minded Syllabus Design Workshop by the Center for Teaching and Learning Excellence. This training prompted her to add detail concerning the weight and purpose of assignments so students would understand what they gain from assessments while increasing motivation.
“Jane is not afraid of challenges. In spring 2022 she taught a two-week immersion travel course in Italy, ‘NSD 452: Mediterranean Food and Culture,’ for the first time. The course was started by a recently retired colleague. When the opportunity arose, Jane jumped at the chance to teach the class, working with Syracuse Abroad to create new student experiences. Jane is excited about modifications for this spring that further enhance the abroad experience.
“Jane strives to provide her students with the most recent evidence-based education. In fact, she is currently enrolled in a Ph.D. program in our very own Human Development and Family Science department. Her list of teaching skills and accomplishments goes beyond what is listed here. On a personal note, I want to add that I am thrilled to be presenting this award to Jane. She was one of the first people I met when I joined Falk and has always been a kind and supportive colleague.”

Lynn Brann
Chair of the departments of Exercise Science and Nutrition and Food Studies, associate professor in the Department of Nutrition and Food Studies
Faculty of the Year Award for Excellence in Service
From presenter Chaya Lee Charles, assistant teaching professor in the Department of Nutrition and Food Studies:
“Lynn has an extensive resume of teaching, research, and service in Falk College and within the University as evidenced by her previous receipt of nine Chancellor’s Awards for public service during her tenure at Syracuse University.
“This academic year, however, she went far above and beyond, accepting her call to duty by chairing not only the combined Department of Nutrition and Food Studies, but also chairing the Department of Exercise Science. Despite this challenging task, Lynn has provided leadership, support, guidance, and advocacy for both departments while mentoring junior faculty in the Nutrition program and assisting Exercise Science faculty and staff through the growing pains of acclimating to Falk College. She has exceeded all expectations one could place on someone assigned such a difficult role and has done so with grace, compassion, understanding, and outstanding professionalism.
“In additional service during 2022 at the University level, Lynn was selected to participate in the inaugural Syracuse University Women in Leadership Cohort Group to support the professional development and career development of women faculty and staff at the University. She also continued her work on the Academic Appeals Committee; the Falk College Promotion and Tenure Committee; the Falk College Diversity, Equity, and Inclusion Committee, and the Falk College Program Review Committee, and she is a Dean’s Cabinet member and serves as a trainer for Academic Integrity panelists and Academic Integrity faculty interviewers.
“Locally, Lynn serves on the Health Services Advisory Board, Peace, Inc., Head Start, and Early Head Start of Syracuse. In her desire to further the profession of nutrition and dietetics, Lynn also serves as advisor to the Pediatric Nutrition Practice Group of the Academy of Nutrition and Dietetics and is a journal reviewer for the Journal of Child and Family Studies, Appetite, Nutrients, the International Journal of Obesity, the Journal of the Academy of Nutrition and Dietetics, the Journal of Nutrition Education and Behavior, Public Health Nutrition, the Journal of the American Medical Association Pediatrics, the Maternal and Child Health Journal, and the Maternal and Child Nutrition Journal.
“I couldn’t be more pleased to honor Lynn with this award as she has been a calming force to our department and a strong leader who consistently considers all aspects of any difficult situation and guides us in the right direction. No matter the problem, she always has an open door and provides sound counsel, such as my favorite piece of wisdom, that ‘It will all be fine!’”

Bryce Hruska
Assistant Professor in the Department of Public Health
Faculty of the Year Award for Excellence in Research
From presenter Lisa Olson-Gugerty, associate teaching professor in the Department of Public Health:
“Over the last several years, Bryce has been systematically building his program of research, investigating post-traumatic stress disorder (PTSD) and its co-occurring mental health consequences, and identifying strategies for addressing PTSD before it takes its full toll on functioning.
“In the past year, he has had several notable accomplishments that have significantly advanced his research program. He submitted six first-authored, peer-reviewed pieces of scholarship resulting in two published peer-reviewed articles, one peer-reviewed article in press, one published peer-reviewed book chapter, and two peer-reviewed articles that are currently under review after receiving an invitation to revise and resubmit. The published/in press pieces all appear in high impact journals, including Sleep Health, Journal of Psychiatric Research, and Journal of Anxiety Disorders.
“Bryce has presented his research and its findings at two international conferences: the International Society for Traumatic Stress Studies and Society for Ambulatory Assessment. These presentations included a peer-reviewed symposium and two peer-reviewed poster presentations.
“Much of his research focuses on the mental health burden experienced by healthcare providers, a topic that has recently received special attention due to the COVID-19 pandemic. To facilitate the translation of his research into practice, this past year he delivered an invited presentation at American Medical Response (the largest ambulance service provider in Central New York) that described his research examining the connection between sleep and mental health. He also wrote two pieces of publicly engaged scholarship–including a blog post and a research brief–that were delivered to an international audience of policy makers, practitioners, media outlets, students, and the public.
“Finally, he was awarded a CUSE Innovative and Interdisciplinary Research Grant supporting the next phase of an intervention that he is developing that will reduce the mental health symptoms experienced by ambulance service providers. This work will serve as pilot data for a subsequent submission for extramural funding from the National Institute of Occupational Safety and Health.
“Collectively, these achievements highlight his commitment to high-quality research that has translational implications and demonstrate the high level of research activity that he has engaged in during the past year. I would like to personally add that as a healthcare worker in emergency medicine who has spent a significant amount of time working in the COVID pandemic, I appreciate all that Bryce has done and continues to do in his research for me and my colleagues.”
Page 7 of 26
